Role
UI development

Claim Middleware is a claim management platform that streamline the entire claims lifecycle for the Sunday claims team. The project was initiated due to the inefficiency of the existing insurance claim process that used multiple spreadsheets and documents to assess incoming claims, track claims processing status, and delegate claim assignments. These issues resulted in longer claim processing times and lower claim processing rates for the claims team.
Sunday's existing claim management system relies on inefficient manual processes, such as spreadsheets and documents. This has led to slow claim processing times, negatively impacting operational efficiency and customer satisfaction.
Prior to the kickoff, we had discussions with the claims team and development director to discuss the plan of improving the existing claim process to be more efficient. We highlighted key pain points of the existing claim process based on the focus group discussions with the team.
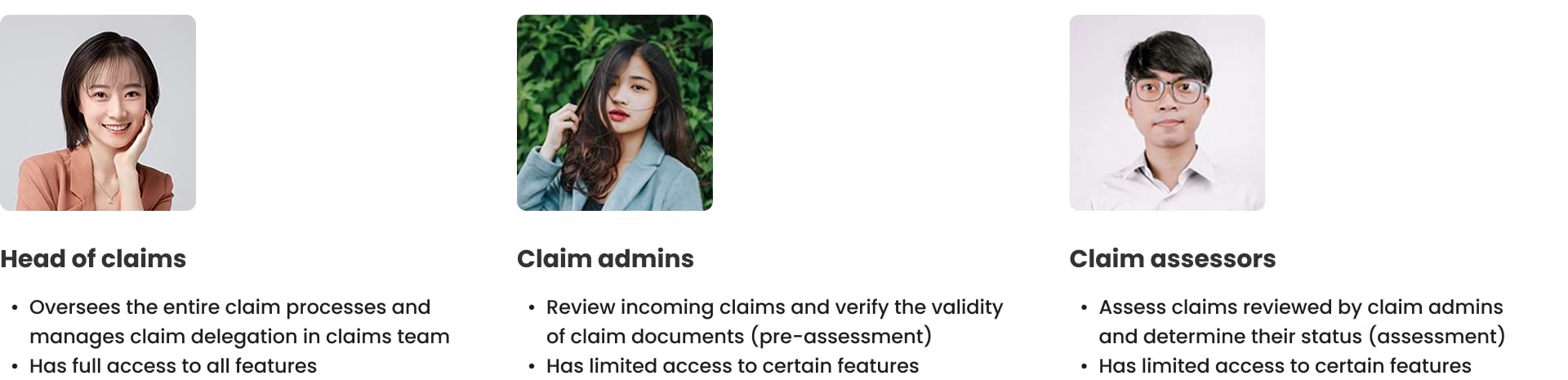
Three distinct user roles will use this platform: claim admins, claim assessors, and heads of claims. Each role will have varying levels of access to platform features.
Our goal was to develop an MVP version of claim management platform for Sunday Insurance, namely Claim Middleware. This platform will streamline the entire claims lifecycle by enabling the Sunday claims team to seamlessly assess incoming claims, track claims processing status, and delegate claim assignments.
My task was to design the end-to-end claim processing workflows from pre-assessment, assessment, to assessment results from scratch. Furthermore, I facilitated team understanding of these complex workflows by providing detailed flows with annotations using charts and diagrams.
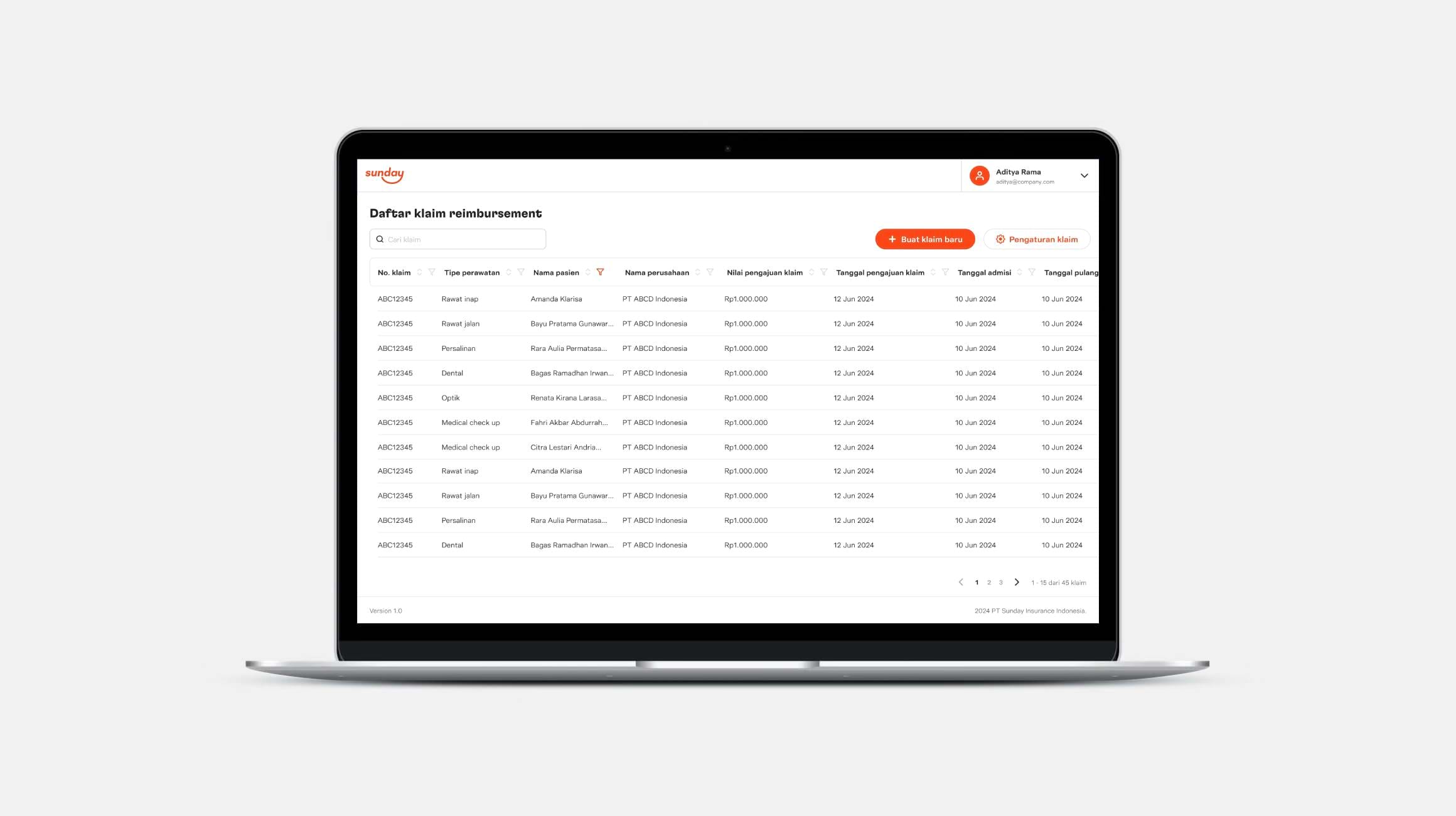 Claim list page, from where the claims team can view the list of submitted claims, add new claims, and adjust claim settings
Claim list page, from where the claims team can view the list of submitted claims, add new claims, and adjust claim settings
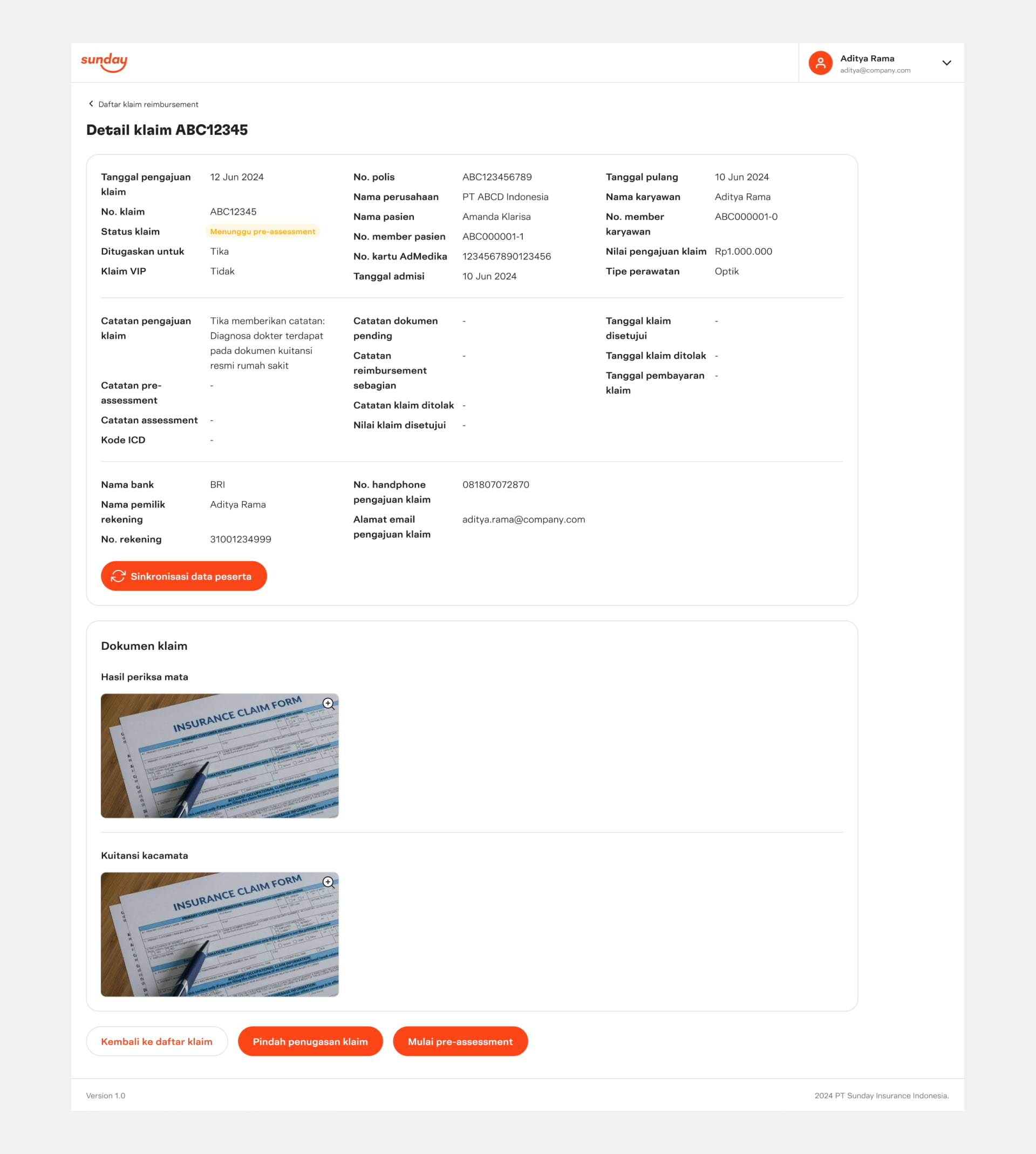 Claim details page, which allows the claims team to review claim information and process the claim
Claim details page, which allows the claims team to review claim information and process the claim
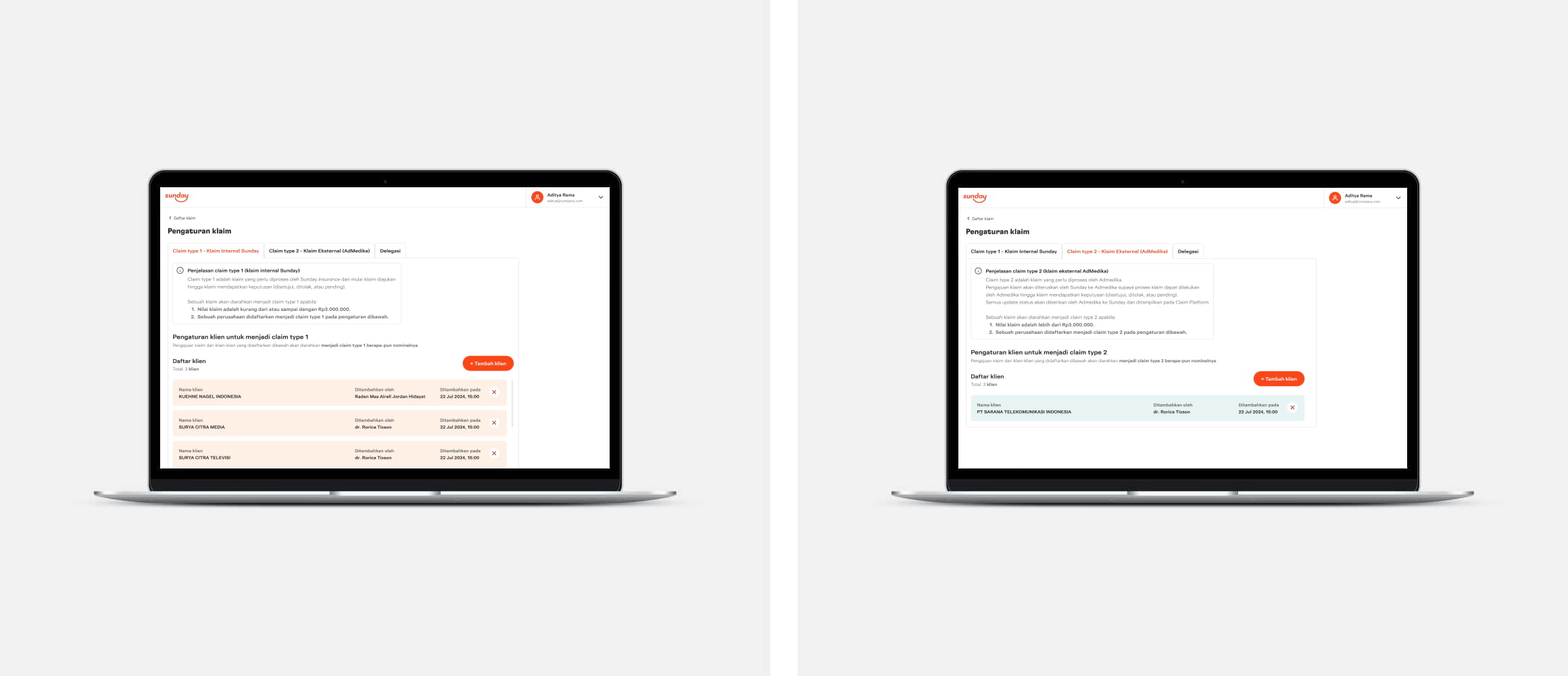 Client configuration, from where clients can be categorized as type 1 (can be processed directly) or 2 (need AdMedika review)
Client configuration, from where clients can be categorized as type 1 (can be processed directly) or 2 (need AdMedika review)
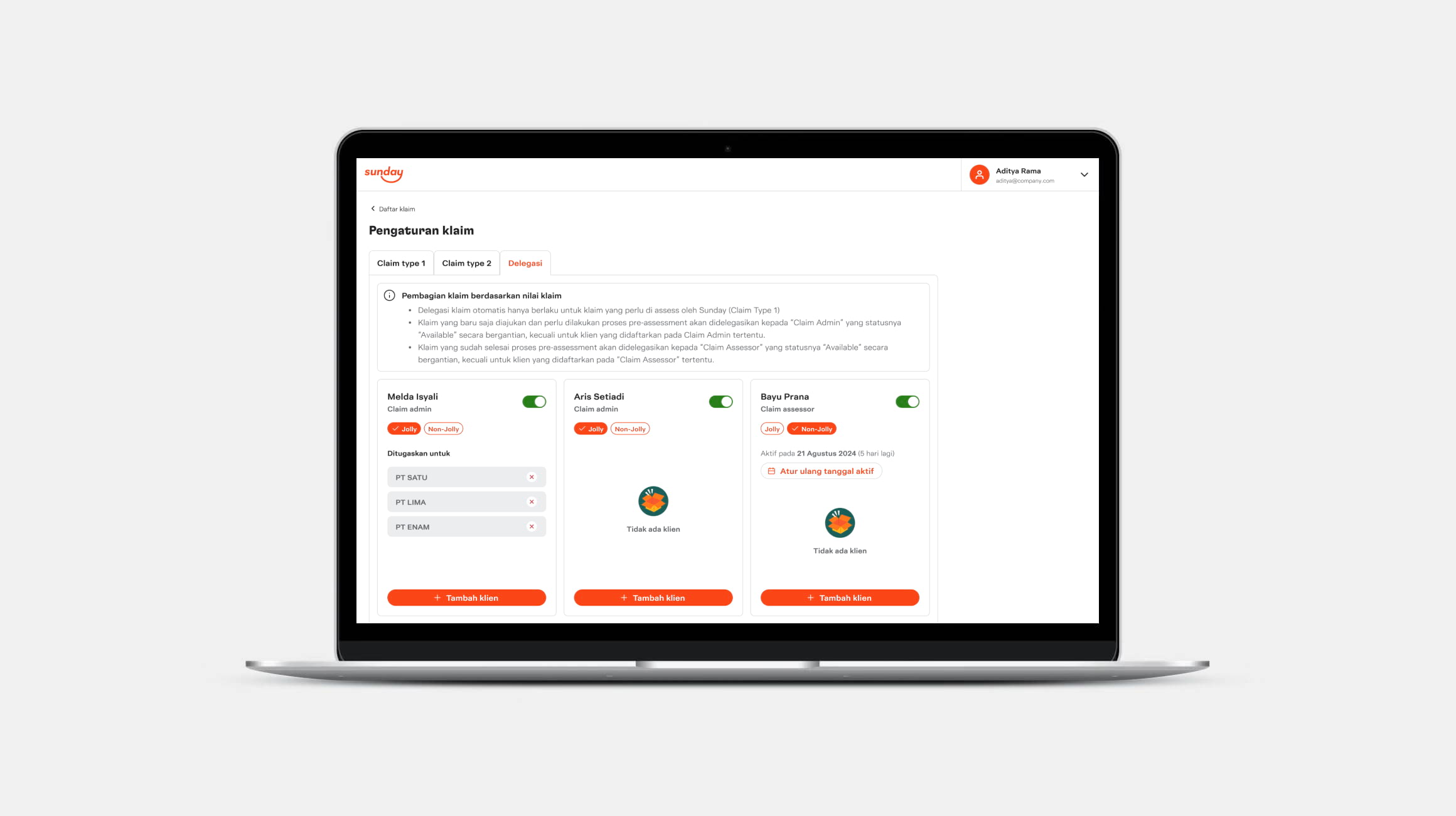 Claim delegation, which was one of the most requested features during the pilot phase
Claim delegation, which was one of the most requested features during the pilot phase
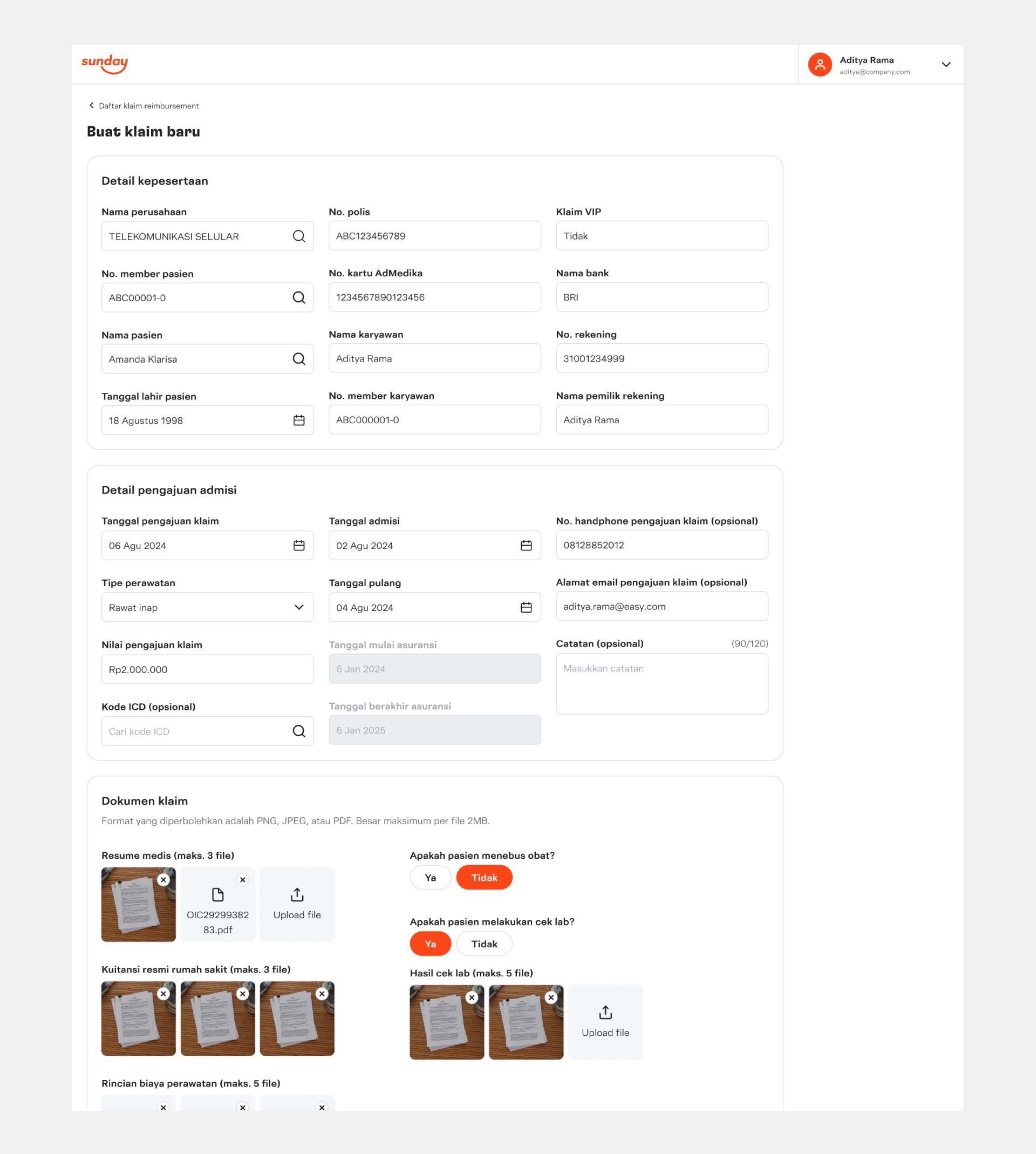 Creating claim, which allows the claims team to create a new claim for instances where claims are submitted outside of Jolly super app
Creating claim, which allows the claims team to create a new claim for instances where claims are submitted outside of Jolly super app
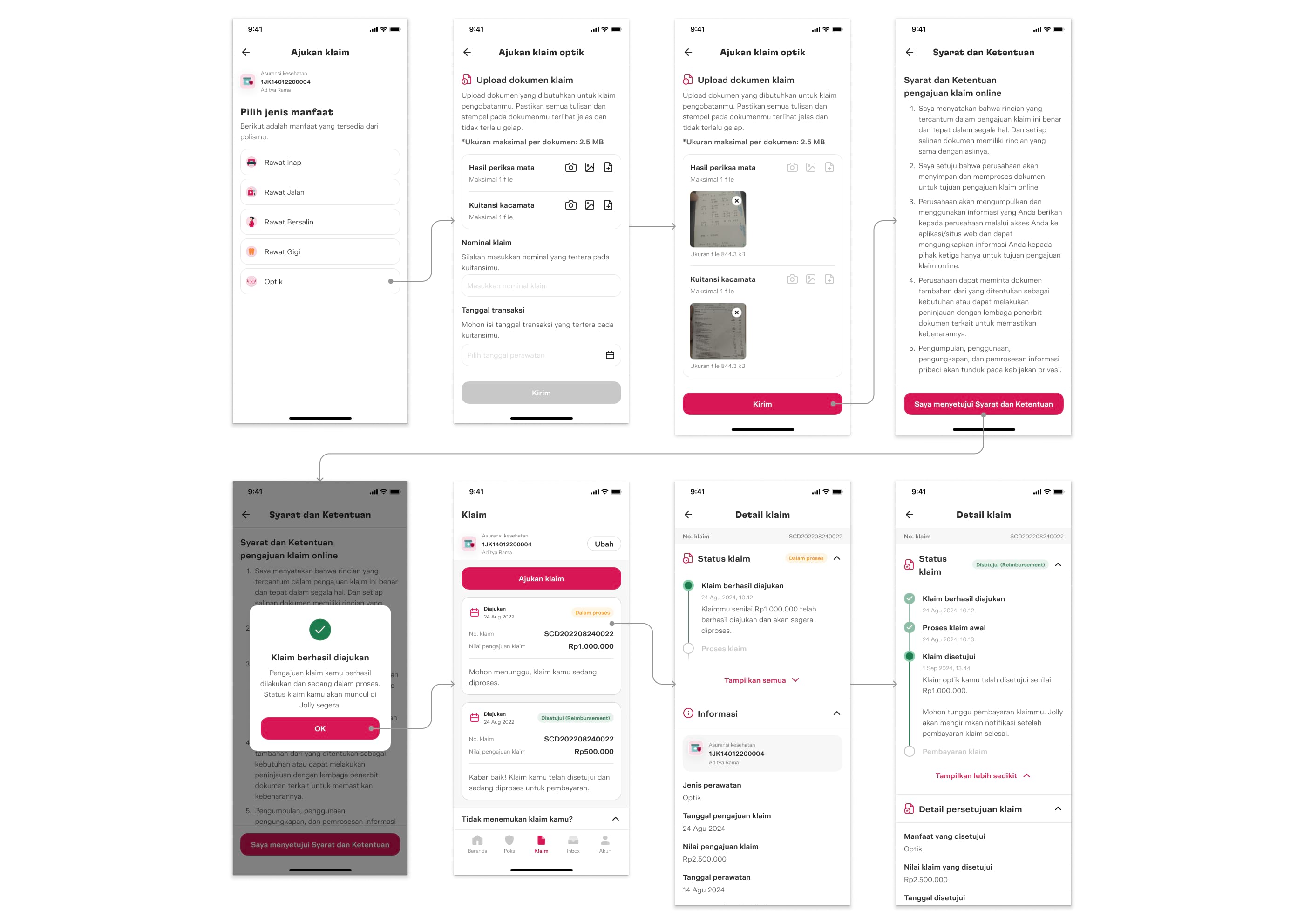 User flow for claim submission via Jolly super app, from submitting a claim to viewing claim history and status
User flow for claim submission via Jolly super app, from submitting a claim to viewing claim history and status